Use the Demographics tab to maintain and update provider information such as the ID, alternate names, how or what information the provider receives, and provider comments and alerts.
- Search for the billing provider.
- In the Provider session, select the
Providermenu and thenBilling Provider Information. -
Select the
Demographicstab.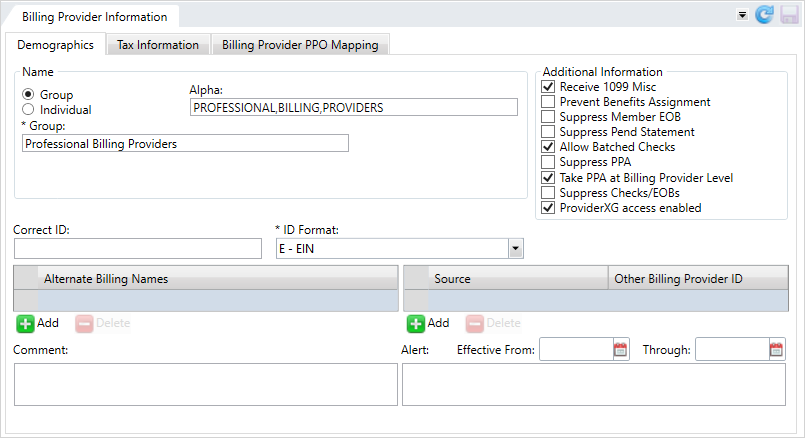
 Billing provider field descriptions
Billing provider field descriptions
* indicates a required field
Name Group/Individual Select either
GrouporIndividualto indicate the provider type.Alpha Auto-updated, read-only field based on the group or individual information entered, used to sort the provider's name in reference lists.
Group The provider group's name. Individual
When the provider isn't in a group these fields apply.
Last Name*—The individual's last name.First Name—The individual's first name.Middle Name—The individual's middle name. You can enter a middle initial rather than a full name.Prefix—A title that displays at the beginning of a person's name to indicate marital status and gender, education, or occupation, (e.g., Dr., Mrs., PhD, etc.)Generation—Suffix to distinguish persons that share the same name in a family, (e.g. Jr., II, Sr, etc.)Select a generation from the list. The list only displays if the System Administrator Control (SAC) is set to perform a data validation on the Generation field.Title—A professional or some other designation that comes at the end of a name, for example, CPA, MD, ESQ, etc. Select a title from the list. The list only displays if the System Administrator Control (SAC) is set to perform a data validation on the Title field.
Additional Information Receive 1099 Misc
Indicates the 1099-MISC form will be sent to the billing provider when it's issued. Prevent Benefits Assignment
Prevent operators from assigning services and benefits to the billing provider. Suppress Member EOB
Prevent generating member EOBs  EOBs are sent to members and payees to inform them of the disposition of claims. Typically an EOB identifies the date and type of service, the billed amount, deductibles, co-insurance, and an explanation of any ineligible charges. An EOB can also be a helpful tool in identifying fraudulent claims, as the member receives notification even when payment is made to the provider. An EOB isn't a bill. when the billing provider is paid.
EOBs are sent to members and payees to inform them of the disposition of claims. Typically an EOB identifies the date and type of service, the billed amount, deductibles, co-insurance, and an explanation of any ineligible charges. An EOB can also be a helpful tool in identifying fraudulent claims, as the member receives notification even when payment is made to the provider. An EOB isn't a bill. when the billing provider is paid.Suppress Pend Statement
Prevent a pend statement being generated for the billing provider. Allow Batched Checks
Indicates that batch multiple claims payable to the billing provider are on one check. Suppress PPA Indicates that the PPA window won't display in claims entry or claims processing when the associated service provider is on the claim.
- Your system might be configured to display suppress the PPA window if the claim is zero.
This field won’t display for the first service provider associated with this billing provider.
If an operator isn't allowed to take PPA (security settings), the PPA window will be suppressed. If the provider or member has a PPA, pend code P28 will be applied to the claim so that an operator who has the ability to determine whether to take PPA or not can complete the claim.
Note: Contact your basys representative to set or change SAC (System Administration Control) settings. Don't change SACs without first consulting basys as changing them can affect other functions and global system settings.Take PPA at Billing Provider Level - If your system is configured to take prior payment adjustments at the service provider level, but this billing provider does not, use this option to have any prior payment adjustments taken at the billing level for any associated service providers.
- If this option isn’t selected and your system is configured to take the prior payment adjustments at the service provider level, the PPA will apply to the service provider and not the billing provider.
Note: Contact your basys representative to set or change SAC (System Administration Control) settings. Don't change SACs without first consulting basys as changing them can affect other functions and global system settings.Suppress Checks/EOBs Indicates that checks and EOBs are suppressed for the billing provider. ProviderXG access enabled Enables user access to the ProviderXG portal. You must select this check box to let Provider contacts access ProviderXG (see Add, update, or delete a provider contact).
Note: If you restrict access to ProviderXG and then enable access again, the contacts previously set up to use the portal on the billing provider's Contacts screen keep their account credentials.Correct ID
The ID to use for this billing provider. A billing provider with this ID must already be in the system.
- Use when bills were originally submitted under this provider ID and were later determined to be incorrect.
ID Format*
The provider ID format.
E—EIN.S—SSN.
Alternate Billing Names
Names other than the billing provider or service provider associated with this billing provider.
Source/Other Billing Provider ID
Other billing provider identifiers along with the source of the ID.
Source—The data source for the other ID.Other Billing Provider ID*—The ID.
Comment
Additional information associated with the provider. Include information that will help other users quickly respond to inquiries about the billing provider. The comment can be up to 50 characters long.
Effective From
Effective Through
Start and end dates for provider alert messages. Click  and select a date or enter a date in
and select a date or enter a date in MM/DD/YYYYformat.Alerts with effective dates only show on a claim when they are within the effective date range.
Alert
Important or critical information about the provider. The alert can be up to 150 characters long.
- The Claims or provider demographics data tile will show an alert icon
 next to the billing provider's name.
next to the billing provider's name. - The alert shows in the Provider Alerts window (if your office is configured that way) and in the Alerts tab when processing a claim associated with the provider. You can add an effective date range to limit the alerts.
- Review the
Nameinformation for the billing provider and update it as needed. See the Billing Demographics Name field descriptions. - In the
Additional Informationarea, choose how claims information will behave with the provider. - If there are any issues with the provider's ID, enter the correct ID that should be used for this billing provider. A billing provider with this ID must already be in the system.
- Select the provider's ID format.
E—EIN (xx-xxxxxxx)S—SSN (xxx-xx-xxxx)
- When you're done updating or adding information, click
 to save.
to save.
To add an alternate billing name:
- Click
 below the
below the Alternate Billing Namesbox. - Click in the field and type the alternate name.
- Press
Enter. - Click
 to save.
to save.
To update an alternate billing name:
- Select the row to update.
- Click in the field and update the alternate name.
- Press
Enter. - Click
 to save.
to save.
To delete an alternate billing name:
- Select the row to delete.
- Click
 below the Alternate Billing Names box.
below the Alternate Billing Names box. - Click
 to save.
to save.
If the billing provider has another identifier, you can enter it here along with the source of the ID.
Source—The data source for the other ID. Select a source from the list.Other Billing Provider ID*—The ID.
To add a source and ID:
- Click
 below the
below the Source/Other Billing Provider IDtable. - Select a source from the list.
- Type the ID and press
Enter. - Click
 to save.
to save.
To update a source and ID:
- Click the
Source/Other Billing Provider IDto update. - Select a different source or update the billing provider ID.
- Press
Enter, then click to save.
to save.
To delete a source and ID:
- Click the
Source/Other Billing Provider IDto delete. - Click
 below the
below the Sourcebox. - Click
 to save.
to save.
Comments help operators respond to inquiries about the billing provider. The comment can be up to 50 characters long. If the provider has a comment, an icon ![]() displays on the provider demographics data tile. Move your cursor over the
displays on the provider demographics data tile. Move your cursor over the ![]() icon to see the complete comment.
icon to see the complete comment.
- Enter, update, or remove the text in the comment box.
- Click
 to save.
to save.
Alerts show while processing a claim, in the alert window (if your system is configured this way). Add alerts for important or critical provider information. Include information operators need to know about the billing provider, like if the billing provider requires special handling. The alert can be up to 150 characters long.
- The Claims or provider demographics data tile will show an alert icon
 next to the billing provider's name. Hover over the icon to see the entire alert text.
next to the billing provider's name. Hover over the icon to see the entire alert text. - The alert shows in the
Provider Alertswindow (if your office is configured that way) and in theAlertstab when processing a claim associated with the provider.
- Enter, update, or remove the text in the
Alertbox. - Click
 to save.
to save.
Set an effective date for provider alerts
You might only need to show a provider alert for a specified time-frame. Instead of remembering to delete the alert, you can set an effective date for the alert. Once the alert is beyond the effective date range, it will no longer display.
- Above the
Alertbox, choose the start and end dates for provider alert message. Click and select a date or enter a date in
and select a date or enter a date in MM/DD/YYYYformat. - Click
 to save.
to save.